
Background: T-cell acute lymphoblastic leukemia (T-ALL) is a rare aggressive neoplasm accounting for ∼20% of all ALL cases. It is more common in adults than in children, although the incidence decreases with older age. Subclassification of T-ALL cases according to WHO is so far solely based on the immunophenotype. Although a number of common molecular aberrations have been described in T-ALL, a molecular classification of T-ALLs so far is missing.
Aim: (1) Molecular subclassification of T-ALL cases based on whole genome sequencing (WGS) and whole transcriptome sequencing (WTS) data. (2) Analysis of correlations between aberrations, subgroups and other parameters.
Methods: WGS and WTS were performed in 114 patients. For WGS, 151bp paired-end reads were generated on NovaSeq 6000 and HiSeqX machines (Illumina, San Diego, CA). For WTS, 101 bp paired-end reads were produced on a NovaSeq 6000 system with a yield between 35 and 125 million paired reads per sample. SPSS (version 19.0.0, IBM Corporation, Armonk, NY) was used for statistical analysis.
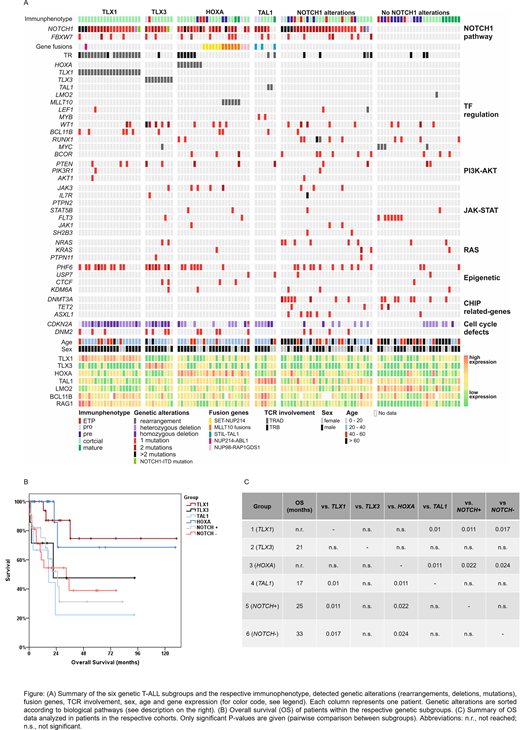
Results: The cohort comprised 114 T-ALL cases (29% female, 71% male) with a median age of 37 years (range 1 - 91 years). Based on mutations (mut), translocations and gene expression, the cases were subdivided into six different groups: group 1 (n=20) was defined by overexpression (oex) of TLX1 (by t(10;14)(q24;q11)/TRAD-TLX1, n=17; t(7;10)(q34;q24)/TRB-TLX1, n=2; inv(10)(q23q24), n=1) and was correlated to a high frequency of mut in NOTCH1 (19/20, 95%, p=0.011 compared to the other T-ALL cases), PHF6 (11/20, 55%, p=0.04) and BCL11B (5/20, 25%, p=0.004). Group 2 (n=9) showed TLX3 oex by t(5;14)(q35;q32)/BCL11B-TLX3 (n=8) or t(5;8)(q35;q24) (n=1). Mut in WT1 (5/9 = 56%, p<0.001) and PHF6 (7/9 = 78%, p=0.005) were frequently detected. Groups 1/2 were further characterized by male predominance (18/20 = 90%, p=0.04 and 8/9 = 89%) and a cortical immunophenotype (20/20 = 100% and 7/9 = 78%). Group 3 (n=23) was defined by oex of HOXA genes, caused by inv(7)(p15q34)/TRB-HOXA (n=6), other HOXA rearrangements (n=2), SET-NUP214 (n=6), NUP98-RAP1GDS1 (n=3) and fusions involving MLLT10 (n=6). Group 4 (n=7) was defined by oex of TAL1 due to the fusion STIL-TAL1 (n=3), t(1;14)(p33;q11)/TRA-TAL1 (n=1), mut in MYB enhancers (n=2) and a MYB-translocation (n=1), and was correlated to the absence of PHF6 mut (p=0.045). The remaining 55 cases did not show oex of TLX1, TLX3, HOXA or TAL1 and were subdivided based on the presence of NOTCH1 aberrations (group 5, n=29, NOTCH1+; group 6, n=26, NOTCH1-). 25/29 NOTCH1+ cases showed at least 1 mut in NOTCH1 (range: 1-3), 2/29 had a t(7;9)(q34;q34)/TRB-NOTCH1, 2/29 showed NOTCH1 deletions. Group 5 correlated to mut in DNMT3A, NRAS and ASXL1 (p=0.001; p=0.006; p<0.001) and comprised a high number of female patients (15/29 = 52%, p=0.004). NOTCH1- cases lacked mut in FBXW7 and DNM2 (p=0.02) and comprised a high number of cases with Pre-T-ALL and mature T-ALL immunophenotype. Other findings include: (1) detection of two cases with a novel type of NOTCH1 mut, termed NOTCH1-ITD, characterized by a duplication event in the NOTCH domain. (2) Mut in DNMT3A, TET2 and ASXL1 were exclusively detected in groups 5 and 6, causing correlation to older age (p=0.011 and p=0.001), whereas the HOXA group was correlated to younger age (p=0.001) (3) NRAS mut were associated with females (6/10 = 60% vs. 27/104 = 26%, p=0.023). (4) Oex of BCL11B and RAG1 was predominantly detected in groups 1 and 4. (5) Mut in DNM2 occurred concomitantly with NOTCH1 mut (p<0.001); NOTCH1 and PHF6 mut were correlated with each other (p=0.008). (6) Female patients were significantly older than male patients (55 vs. 36 years, p=0.005). (7) Finally, analysis of OS (total cohort median: 36 months (m)) in the six groups revealed a significantly more favorable outcome of groups 1 (TLX1; n.r.) and 3 (HOXA; n.r.) compared to the other groups (see table), which might be linked to the high number of cases with cortical immunophenotype.
Conclusions: (1) The combination of WGS and WTS successfully subclassified T-ALL cases on a molecular level into six different groups, by oex of TLX1, TLX3, HOXA or TAL1 and presence/absence of NOTCH1 mut. (2) We identified a novel so far unknown type of NOTCH1 aberrations, termed NOTCH1-ITD. (3) Molecular sub-classification of T-ALL cases also impacts on prognosis (TLX1 and HOXA group, longer OS; NOTCH1+ and TAL1 group, shorter OS).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal